Uveitis is inflammation of the uveal layer. This is the middle layer of the three that make up the eye. Their are several different forms of Uveitis. These forms can affect the retina, iris and in extreme conditions can affect the optic nerve. Uveitis can be caused by a multitude of conditions. These include: eye surgery, eye cancer and possibly a side effect of an underlying condition. Uveitis could be indicated by blurred vision, pain in the eyes and red eyes. Eye drops are a treatment option for Uveitis, but are not always successful if they don't penetrate to the back of the eye. Injections to the eye, oral medications and even surgical procedures are ways to combat Uveitis. Uveitis can be treated in a couple months in mild conditions. However, in severe cases, the Uveitis can last quite a while.
My name is Erica Loesel and I am a senior Co-Op at Auburn Optical. Check out all of the extraordinary projects I had the opportunity to complete during my amazing year working here!
Thursday, January 31, 2019
Thursday, January 17, 2019
Thursday, January 3, 2019
Diplopia
Diplopia is the technical term for double vision. This condition is when you see two images that could either be side by side or on top of each other. Diplopia can occur is both eyes or just a single eye. Diplopia in only one eye could be caused by cornea damage and can be fixed with the use of glasses. Lens issues such as cataracts can also be a cause of diplopia in a single eye. Surgery is the main treatment for cataracts. Diplopia in both eyes can be caused by issues within the muscles of your eye, nerves and even your brain. Conditions such as Diabetes, Graves' Disease, and even having a stroke can cause you to have double vision.
Symptoms of Diplopia include misalignment of your eyes, pain, headaches, nausea and even droopy eyelids. Diagnosis of double vision can be performed by your regular eye doctor. You could eventually have more testing including: blood tests, a physical exam and possibly even a CT scan. Surgery and medication are the most common treatments for diplopia. The treatment for double vision really depends on what caused the double vision in the first place. If the Diplopia does not go away after these treatments, their are a couple other options. Glasses, prisms, and eye patching are all forms of treatment for Diplopia to help you live with condition.
Symptoms of Diplopia include misalignment of your eyes, pain, headaches, nausea and even droopy eyelids. Diagnosis of double vision can be performed by your regular eye doctor. You could eventually have more testing including: blood tests, a physical exam and possibly even a CT scan. Surgery and medication are the most common treatments for diplopia. The treatment for double vision really depends on what caused the double vision in the first place. If the Diplopia does not go away after these treatments, their are a couple other options. Glasses, prisms, and eye patching are all forms of treatment for Diplopia to help you live with condition.
Thursday, December 27, 2018
Wednesday, November 28, 2018
Keratitis
Today I had the opportunity to do some research on Keratitis. Keratitis is inflammation of the cornea that can be caused by different types of infections, dry eye, and injuries to the eye. Symptoms of this condition include: eye redness, eye pain, blurred vision, and sensitivity to lights. There are some major risk factors that go along with keratitis. Sleeping in your contact lenses and having a compromised immune system increases your chance of obtaining keratitis. There are some ways to prevent keratitis. Washing your hands before handling your contacts is key to a healthy eye. When you are sick, avoid touching your eyes so you don't spread an infection. I am very grateful too have had the opportunity to research this eye condition.


Tuesday, November 20, 2018
November Project on Amblyopia
Tuesday, November 13, 2018
I had the opportunity to research some information on History of Present Illness. Read below for what I found out!
HPI Notes
1. Chief Complaint
a. Reason why the patient has come to see the doctor
b. Don’t ask questions robotically
i. Smile and talk to the patient J
2. History of Present Illness
a. Gather details about chief complaint
i. Qualify and quantify
b. Location
i. Where? What part of eye?
c. Quality
i. Sharp or dull pain?
d. Severity
i. Unbearable pain or mild?
e. Duration
i. Suddenly or gradually?
f. Timing
i. Constant or comes and goes?
g. Context
i. What were you doing when it happened?
h. Modifying Factors
i. Have you done anything to help?
i. Signs
i. Noticed anything additional?
3. Review of Symptoms
a. Cardiovascular, vasucalar, respiratory, etc.
b. Always record patients answer, otherwise it is taken like it was not asked
4. Past Medical Histories
a. Ask about eye surgeries
b. Document these!
i. High blood pressure
ii. Diabetes
5. Medications
a. Blood thinning medications
i. Ask, could lead to explanation for brain bleed etc.
b. Review current Medications
i. See if any have stopped or changed
c. Record over the counter medications
i. Vitamins and meds
d. Compliance
i. See if they have actually been takin medication
6. Drug Allergies
a. Record what patient is allergic to
i. Include reaction and whether it is severe or not
7. Family History
a. Always ask about these
i. Glaucoma, macular degeneration, retinal detachment, amblyopia, hypertension, diabetes and cataracts
8. Social History
a. Ask about alcohol, drugs, and tobacco
i. Can be VERY awkward
9. Pertinent Questions
a. Specific questions to type of visit
b. Put in HPI answers to questions regarding the symptom
10. HIPAA
a. Health Insurance Portability and Accountability Act of 1996
i. Shred patient info, do not talk loud about patient, don’t leave files visible to others
11. Triage
a. Emergency Situation
i. Result from pain, redness, blurred vision
12. Documentation
a. Age, sex, and race
b. Mood and orientation
13. Questions to Ask Per Appointment
a. Cataracts
i. Glare or blurry vision
ii. Have you had surgery?
b. Glaucoma - New Patient
i. How long?
ii. Eye drops?
iii. Who diagnosed it?
c. Glaucoma – Established Patient
i. Eye pain or redness?
ii. Using drops as instructed?
d. Retina Problems
i. Family History?
ii. When have you noticed changes?
iii. Both eyes or one?
e. Diabetic Exam
i. A1C Value?
ii. Fasting Blood Sugar Level?
iii. Well controlled?
f. Droopy Eyelids
i. Any surgeries?
ii. Double Vision?
g. Trauma
i. Wearing safety glasses?
ii. Occur on the job?
iii. Date and time?
iv. How did it happen?
h. Contact Lenses
i. What kind?
ii. Bifocal?
iii. How many hours a day?
iv. Sleeping in lenses?
v. How many years have you been wearing them?
vi. Last time you wore them?
vii. Solutions you use?
In summary, when evaluating a patient, play the detective role. Figure out what their problem is and why they are experiencing it. Always ask the small details and input that information into the HPI. Above all, be friendly and maintain a certain level of professionalism.
Subscribe to:
Posts (Atom)
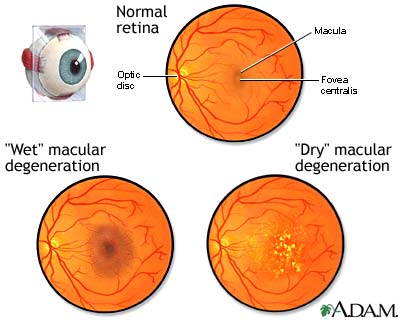
Macular Degeneration
Today I had the opportunity to research macular degeneration. Macular Degeneration is caused by the deterioration of the part of the retina ...
-
Today I had the opportunity to research macular degeneration. Macular Degeneration is caused by the deterioration of the part of the retina ...
-
Click on the video below to watch me present on tsunamis! Also follow this link to check out my slideshow presentation! http://prezi.com/2m...
-
Today I had the opportunity to do some research on Keratitis. Keratitis is inflammation of the cornea that can be caused by different types ...